Pilonidal Sinus Infection: Causes, Symptoms, and Treatment Options
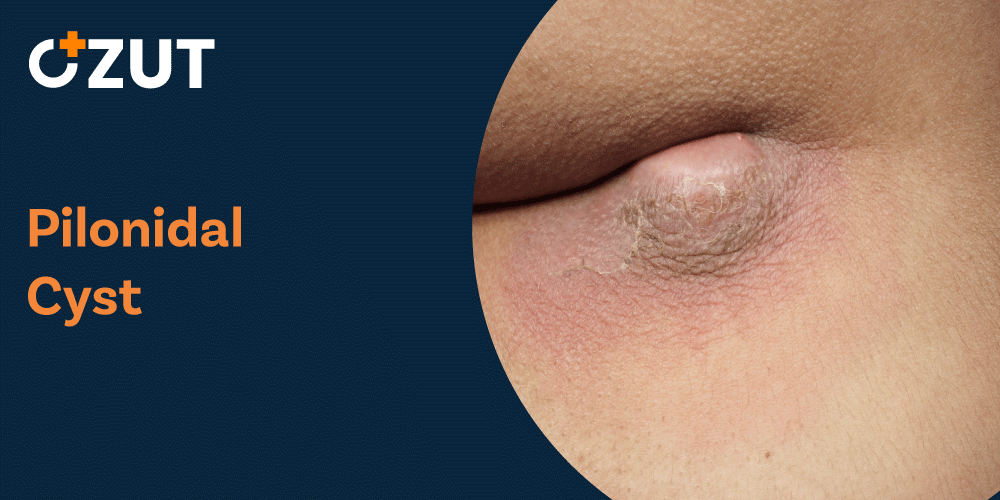
A pilonidal sinus is a small hole or tunnel that develops in the skin, typically forming in the cleft at the top of the buttocks. This condition can become problematic when infected, transforming into a painful abscess or cyst. Understanding this condition is crucial for early detection and proper treatment, especially since it affects many young adults and individuals with sedentary lifestyles.
What Is a Pilonidal Sinus?
The term “pilonidal” comes from Latin, meaning “nest of hair.” This accurately describes the condition, as a pilonidal sinus often contains hair, dirt, and debris. When infected, these sinuses can cause severe pain, discharge pus and blood, and emit a strong, unpleasant odor.
This condition predominantly affects men and is particularly common in young adults. People who spend extended periods sitting, such as office workers or professional drivers, have a higher risk of developing this condition. The prevalence among these groups highlights the role that pressure and friction play in its development.
Understanding the Causes of Pilonidal Sinus
While the exact cause of pilonidal sinus infections remains somewhat unclear, medical professionals believe several factors contribute to their development:
Hormonal Changes
The condition typically appears after puberty, suggesting that hormonal changes play a significant role. These hormonal shifts can affect hair growth patterns and skin characteristics in the affected area.
Hair Growth and Ingrown Hairs
The presence of hair in the gluteal cleft is a primary factor. When loose hairs penetrate the skin, the body treats them as foreign objects, triggering an immune response similar to how it would react to a splinter.
Friction and Pressure
Activities that create friction in the buttock area, particularly prolonged sitting, can force hair to burrow back under the skin. This mechanical pressure is especially relevant for those with occupations requiring extended periods of sitting.
Anatomical Factors
Some individuals may have anatomical features that make them more susceptible, such as deep gluteal clefts or particular hair growth patterns. These physical characteristics can increase the likelihood of hair becoming embedded in the skin.
Recognizing the Symptoms
Pilonidal sinus infections develop progressively, often beginning with subtle signs before evolving into more painful and obvious symptoms.
Early Signs
Initially, you might notice only a small, dimple-like depression on the surface of your skin at the top of the buttock cleft. This early stage may be asymptomatic or cause only mild discomfort.
Infection Symptoms
Once infection sets in, the condition rapidly progresses. The depression develops into either a cyst (a closed sac filled with fluid) or an abscess (swollen, inflamed tissue containing pus). At this stage, several distinct symptoms become apparent:
- Intense pain when sitting or standing
- Noticeable swelling in the affected area
- Reddened, tender skin surrounding the site
- Drainage of pus or blood with a characteristic foul odor
- Visible hair protruding from the lesion
- Development of multiple sinus tracts or holes in the skin
Some patients may experience a low-grade fever, though this is less common than the other symptoms. The combination of pain, swelling, and drainage often prompts individuals to seek medical attention, as these symptoms can significantly impact daily activities and quality of life.
Diagnosis Process
Healthcare providers typically diagnose a pilonidal sinus through physical examination. During this assessment, the doctor will examine the affected area for characteristic signs such as openings in the skin, inflammation, and the presence of hair within the sinus tract.
In some cases, additional tests may be ordered to rule out other conditions or to assess the extent of the infection. These might include blood tests to check for elevated white blood cell counts (indicating infection) or imaging studies in complex cases.
Treatment Approaches for Pilonidal Sinus
Treatment options range from conservative management to surgical intervention, depending on the severity of the condition and whether it’s a first occurrence or a recurrent problem.
Conservative Treatment
For early-stage cases with minimal symptoms and no significant inflammation, healthcare providers often begin with conservative approaches. These typically include:
- Prescription of broad-spectrum antibiotics to address the bacterial infection
- Recommendations for regular hair removal around the affected area
- Guidance on proper hygiene practices to prevent worsening of the condition
It’s important to understand that while conservative treatment can alleviate infection and discomfort, it doesn’t heal the sinus tract itself. Regular follow-up appointments are essential to monitor progress and determine if additional interventions are necessary.
Lancing Procedure
When a pilonidal abscess forms, a procedure called lancing may be performed to provide immediate relief. This procedure involves:
- Administration of local anesthetic to numb the area
- Making an incision with a scalpel to open the abscess
- Thorough cleaning to remove hair, blood, and pus from inside
- Packing the wound with sterile dressing
After lancing, the wound is left open to heal from the inside out, a process that typically takes about four weeks. Many patients find that this procedure provides sufficient treatment and don’t require further interventions.
Phenol Injection Therapy
Another treatment option involves injecting phenol, an antiseptic chemical compound, into the cyst after administering local anesthesia. This approach may require multiple sessions and works by causing the lesion to harden and eventually close.
However, phenol injection has a high recurrence rate and is therefore not commonly used in some countries where surgical approaches are preferred. The effectiveness varies significantly between patients, making it a less predictable treatment option.
Surgical Interventions
For recurring infections or cases with multiple sinus tracts, surgical treatment becomes the preferred approach. Surgical procedures for pilonidal sinus typically involve:
- Administration of anesthesia (local or sometimes general)
- Opening the lesions to access the affected tissue
- Complete removal of all infected material, debris, and hair
- Either closing the wound with stitches or leaving it open to heal, depending on the specific technique used
Post-surgical care instructions typically include guidance on changing dressings and recommendations for regular hair removal to prevent recurrence. The recovery period varies based on the specific surgical technique employed.
Recovery and Healing Timeline
The healing time for a pilonidal sinus infection varies depending on the severity of the condition and the treatment approach. Generally, patients can expect:
- 4-10 weeks for complete healing following treatment
- Shorter recovery periods for conservative treatments and lancing
- Longer recovery times for extensive surgical procedures
During recovery, patients are typically advised to avoid prolonged sitting and to maintain meticulous hygiene in the affected area to promote healing and prevent complications.
Potential Complications
Despite appropriate treatment, complications can occur with pilonidal sinus infections. The most common complications include:
Wound Infection
Signs of post-treatment wound infection include:
- Severe, increasing pain
- Pronounced inflammation and swelling
- Fever of 100.4°F (38°C) or higher
- Purulent drainage with blood from the wound
- Foul odor emanating from the treatment site
Recurrence
Even after successful treatment, pilonidal sinus infections can recur. The recurrence rate varies depending on the treatment method, with some surgical techniques offering lower recurrence rates than others. Patients with recurring infections may need to consider more definitive surgical approaches.
Prevention Strategies
Preventing pilonidal sinus infections involves addressing the factors that contribute to their development. Effective preventive measures include:
Proper Hygiene
- Washing the gluteal cleft area daily with mild soap
- Ensuring all soap is thoroughly rinsed away
- Keeping the area completely dry after bathing
Hair Management
- Regular removal of hair in the affected area through shaving, waxing, or other depilatory methods
- Professional hair removal treatments for those with recurring infections
Lifestyle Adjustments
- Avoiding prolonged sitting when possible
- Using cushions designed to reduce pressure on the tailbone area
- Taking regular breaks to stand and move around, especially for those with sedentary occupations
- Maintaining a healthy weight to reduce pressure on the gluteal region
When to Seek Medical Attention
While some minor cases might resolve with home care, certain symptoms warrant prompt medical evaluation. Seek healthcare if you experience:
- Increasing pain in the tailbone area
- Noticeable swelling or redness
- Drainage of pus or blood
- Fever accompanying other symptoms
- Recurrent episodes of infection
Early intervention can prevent the condition from worsening and may allow for less invasive treatment options. Remember that while pilonidal sinus infections can be uncomfortable and embarrassing, they are a common medical condition that healthcare providers routinely treat.
Conclusion
Pilonidal sinus infections represent a challenging but manageable condition that affects many individuals, particularly young adult males and those with sedentary lifestyles. Understanding the causes, recognizing the symptoms, and knowing the available treatment options empowers patients to seek appropriate care and take preventive measures.
With proper treatment and preventive strategies, most people can effectively manage this condition and minimize its impact on their daily lives. For recurrent or severe cases, consulting with a healthcare provider specializing in this area can help determine the most appropriate treatment approach for long-term resolution.