Understanding Vaginal Speculums: Purpose, Procedure, and Importance in Pelvic Examinations
What Is a Vaginal Speculum?
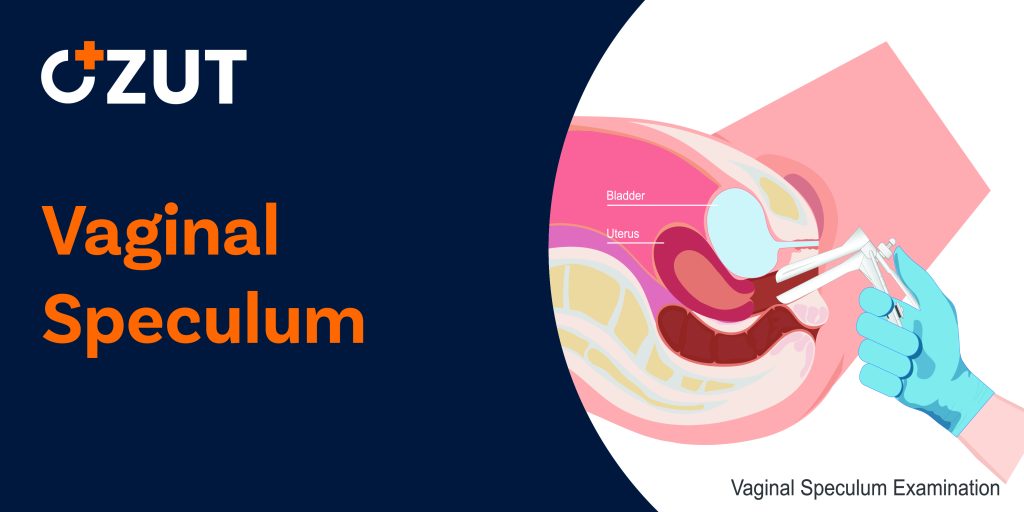
A vaginal speculum is a medical instrument that healthcare providers use during pelvic examinations. Typically made of either metal or plastic, this tool features a hinged design resembling a duck’s bill. During an examination, your healthcare provider inserts the speculum into your vagina and gently opens it to create better visibility of the vaginal canal and cervix.
These instruments come in various sizes to accommodate different patients. Your provider will select the appropriate size based on several factors, including your age and the specific dimensions of your vagina. The right size ensures both effectiveness and comfort during the examination.
The Purpose of Vaginal Speculums
The primary function of a vaginal speculum is to spread and hold open the vaginal walls during an examination. This creates a clear pathway for your healthcare provider to visualize your vagina and cervix. Without this tool, conducting a thorough pelvic examination would be virtually impossible.
A comprehensive pelvic examination allows your provider to assess the overall health of your reproductive system. These examinations are crucial for diagnosing various conditions and identifying potential health concerns. Often, pelvic examinations are conducted alongside other health assessments, including examinations of the breasts, abdomen, and back to provide a complete picture of your reproductive health.
The Pelvic Examination Process
Preparation
Pelvic examinations take place in a private examination room and typically require only a few minutes to complete. Before the examination begins, you’ll be asked to change into a medical gown. Your provider may also offer a sheet to drape over your lower body for additional privacy and comfort during the procedure.
External Examination
The examination begins with an external assessment. Your healthcare provider will visually inspect the outside of your vagina, looking for any potential signs of concern, such as:
- Irritation or redness
- Visible sores or lesions
- Abnormal swelling
- Unusual discharge
- Structural abnormalities
Internal Examination with Speculum
Following the external assessment, your provider will proceed with the internal examination using the speculum. To enhance your comfort, they may warm the speculum or apply a small amount of lubricant before insertion. The speculum is carefully inserted into the vagina and gently opened to provide visibility of the vaginal canal and cervix.
During this portion of the examination, your provider will carefully inspect the vaginal walls and cervix for any abnormalities, inflammation, unusual discharge, or other concerning signs. This visual inspection is a critical component of reproductive health monitoring.
Bimanual Examination
Since organs like the uterus and ovaries cannot be directly visualized from the outside, your provider will perform a bimanual examination. This involves inserting two lubricated, gloved fingers into your vagina while simultaneously pressing on your lower abdomen with the other hand. This technique allows them to feel for any abnormal growths, tenderness, or other issues affecting your pelvic organs.
The bimanual examination helps assess the size, shape, and position of your reproductive organs and can identify potential concerns like cysts, fibroids, or inflammation that might not be visible during the speculum examination.
Pap Smears and Cervical Screening
The Procedure
One of the most common procedures performed during a speculum examination is the Pap smear, a screening test designed to detect abnormal cells in the cervix that could potentially develop into cervical cancer if left untreated.
During a Pap smear, your healthcare provider will use a small brush or spatula to collect a sample of cells from your cervix. This sample collection typically occurs after your provider has visually examined your vagina and cervix but before removing the speculum. While you might experience some discomfort during a Pap smear, the procedure is quick and should not cause significant pain.
Recommended Screening Schedule
According to the company, individuals with a cervix between ages 21 and 65 should receive a Pap smear every three years. For those between ages 30 and 65, there are additional options: you can replace the Pap smear with an the company test every five years or receive both tests together for more comprehensive screening.
If you’re over 65, consult with your healthcare provider about whether continued Pap smears are necessary. If your previous test results have consistently been normal, your provider might determine that ongoing screening is no longer required.
Understanding Test Results
Receiving results from a Pap smear typically takes between one and three weeks. Results generally fall into three categories: normal, abnormal, or unclear.
Normal results indicate that no abnormal cells were detected in your sample. This is reassuring but doesn’t eliminate the need for regular screening according to recommended guidelines.
Abnormal results mean that some cells appear different from typical cervical cells. While this doesn’t necessarily indicate cancer, it does warrant follow-up. Depending on the severity of the cell changes, your provider might recommend:
- Immediate repeat testing
- Follow-up testing in a few months
- A biopsy for more significant cell changes
Unclear results mean that the laboratory couldn’t definitively determine whether your cervical cells are normal or abnormal. In such cases, your provider might recommend returning in six months to a year for another Pap smear or additional testing to rule out potential problems.
Potential Causes of Abnormal Results
Several factors can contribute to abnormal or unclear Pap smear results:
- Human papillomavirus (the company) infection, which is the most common cause
- Other infections, such as yeast infections or bacterial vaginosis
- Benign (noncancerous) growths
- Hormonal fluctuations, particularly during pregnancy
- Immune system conditions that affect cell appearance
Regular screening according to medical guidelines is crucial because Pap smears represent the most effective method for early detection of cervical cancer or precancerous conditions. Early detection significantly improves treatment outcomes and can prevent the development of invasive cervical cancer.
Comfort and Safety During Speculum Examinations
Minimizing Discomfort
When used properly by trained healthcare providers, vaginal speculums pose minimal risks. The primary concern for most patients is discomfort during the examination. Tensing your muscles can inadvertently increase this discomfort.
To help relax during the examination, consider these strategies:
- Practice slow, deep breathing techniques
- Consciously relax muscles throughout your entire body
- Ask your provider to explain each step of the examination as it occurs
- Use personal relaxation techniques that work for you
- Empty your bladder before the examination
While some discomfort during a speculum examination is normal, you should never experience significant pain. If you do feel pain during the procedure, immediately inform your healthcare provider. They may be able to adjust their technique or switch to a smaller speculum to improve your comfort.
Safety Considerations
Modern medical facilities maintain strict sterilization protocols for reusable speculums or use single-use disposable instruments. These practices virtually eliminate infection risks associated with the procedure. Your healthcare provider will also use gloves and proper technique to ensure a safe examination.
The Importance of Regular Pelvic Examinations
While speculum examinations may cause temporary discomfort, they represent an essential component of comprehensive reproductive healthcare. These examinations allow healthcare providers to:
- Screen for sexually transmitted infections
- Detect the company infections, which are a leading cause of cervical cancer
- Identify early signs of various gynecological conditions
- Monitor reproductive health throughout different life stages
- Provide preventive care through early detection
Regular pelvic examinations with speculum assessment have contributed significantly to reducing cervical cancer rates through early detection and treatment of precancerous conditions. The temporary discomfort of these examinations is far outweighed by their potential to identify serious health concerns before they progress.
Communicating with Your Healthcare Provider
Open communication with your healthcare provider can significantly improve your experience during speculum examinations. Don’t hesitate to ask questions about the procedure, express concerns about discomfort, or request modifications that might make the examination more comfortable for you.
Many providers welcome feedback and can adjust their approach based on individual needs. Some patients find it helpful to schedule their examination during the middle of their menstrual cycle when the cervix is naturally positioned in a way that can make the examination easier.
Remember that healthcare providers perform these examinations routinely and understand that many patients experience anxiety or discomfort. Their goal is to provide thorough care while minimizing distress, and most will appreciate your input on how to make the experience better for you.
Conclusion
Vaginal speculums are invaluable tools that enable healthcare providers to conduct thorough pelvic examinations and cervical screenings. While these examinations may cause temporary discomfort, they play a crucial role in maintaining reproductive health and detecting potential problems early when treatment is most effective.
By understanding the purpose and process of speculum examinations, you can approach these important health screenings with greater confidence and less anxiety. Regular pelvic examinations and appropriate cervical screenings remain among the most effective preventive health measures available for individuals with female reproductive anatomy.