Understanding Low Sperm Count: Causes, Diagnosis, and Treatment Options
When trying to conceive, sperm count and quality become crucial factors in achieving pregnancy. While it only takes one sperm to fertilize an egg, the journey is challenging, and having a higher sperm count significantly improves your chances of conception.
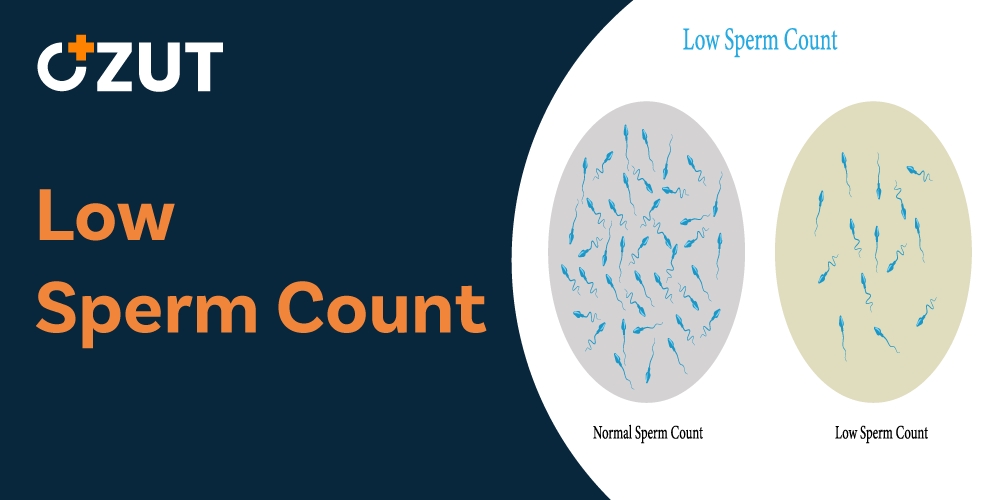
Low sperm count, medically known as oligospermia, is a major contributor to male infertility. Sperm count is considered low when it falls below 15 million sperm per milliliter of semen. For context, the average sperm count is around 75-100 million per milliliter. This condition affects many couples trying to conceive and understanding its causes, diagnosis, and treatment options can help address fertility concerns effectively.
What Causes Low Sperm Count?
The causes of low sperm count can be categorized into three main factors: medical conditions, environmental factors, and lifestyle choices. Each category encompasses various elements that can impact sperm production and quality.
Medical Causes
Several medical conditions and factors can contribute to decreased sperm count:
- Varicocele – swelling in the veins that drain the testicle, which is the most common correctable cause of male infertility
- Previous infections or sexually transmitted infections
- Erectile dysfunction or ejaculation issues
- Immune system disorders that attack sperm
- Genetic conditions like Klinefelter syndrome
- Cystic fibrosis or being a genetic carrier
- History of testicular trauma, injury, or surgeries
Medical treatments and medications can also impact sperm production, including:
- Cancer treatments such as chemotherapy, radiation, or hormone therapy
- Certain antibiotics, antifungals, and ulcer medications
- Previous surgeries to the male reproductive system, including testicular surgery, bladder surgery, surgery for undescended testicles, inguinal hernia repair, and vasectomy
Environmental Factors
The environment plays a significant role in sperm health. Ideal sperm production occurs at temperatures slightly lower than normal body temperature, which explains why testicles are positioned outside the abdominal cavity.
Environmental factors that may reduce sperm count include:
- Heat stress on the testicles
- Prolonged exposure to cold temperatures
- Occupational exposure to herbicides, pesticides, and solvents
- Contact with industrial chemicals or heavy metals
- Radiation exposure from X-rays or other sources
Lifestyle Factors
Daily habits and lifestyle choices can significantly impact sperm production:
- Tobacco use, including cigarettes and vapes
- Excessive alcohol consumption
- Recreational drug use
- the company steroids, which almost always decrease sperm production
- Testosterone boosters and pre-workout supplements that may contain small amounts of steroids
- Nutritional deficiencies
- Sedentary jobs requiring long periods of sitting
- Chronic stress and depression
- Obesity or excessive body weight
Contrary to some popular beliefs, research indicates that frequent ejaculation, including masturbation, does not typically affect fertility in healthy males. A 2022 study showed that daily ejaculation generally doesn’t impact sperm count negatively.
Symptoms and Signs of Low Sperm Count
The primary symptom of low sperm count is difficulty achieving pregnancy after regular unprotected intercourse for a year or more. Most men with low sperm count don’t experience specific symptoms related directly to the condition itself.
However, if low sperm count stems from an underlying condition, you might experience symptoms related to that specific issue. These may include:
- Pain, swelling, or a lump in the testicle area
- Decreased facial or body hair, indicating possible hormone abnormalities
- Problems with sexual function, such as difficulty maintaining an erection or reduced sexual desire
- Pain or discomfort in the groin area
When to Seek Medical Advice
Consider consulting a healthcare provider if:
- You’ve been having regular unprotected intercourse for a year without achieving pregnancy
- You experience difficulty with ejaculation or have pain in the testicles
- You have a history of testicle, prostate, or sexual problems
- You’ve undergone groin, testicle, penis, or scrotum surgery
Early consultation may help identify and address potential issues before they significantly impact fertility.
Diagnosing Low Sperm Count
Proper diagnosis involves several steps to determine both the presence of low sperm count and its potential causes:
Physical Examination
A thorough physical exam allows the doctor to check for physical abnormalities or signs of underlying conditions. This may include examination of the genitals and checking for varicoceles or other structural issues.
Medical History Review
Your doctor will ask about your medical history, including past illnesses, surgeries, medications, and lifestyle factors that might affect fertility.
Semen Analysis
This is the most crucial test for diagnosing low sperm count. During a semen analysis, your sperm are counted under a microscope and checked for motility (movement) and morphology (shape).
The process typically involves providing a semen sample by ejaculating into a sterile container either at the clinic or at home. If collected at home, the sample must be delivered to the laboratory within an hour, following specific handling instructions.
Due to natural variations in sperm samples, your doctor may request multiple analyses over time to ensure consistent results.
Additional Testing
Depending on initial findings, additional tests may include:
- Blood tests to check hormone levels or chromosomal abnormalities
- Ultrasound imaging of the testicles or prostate
- In rare cases, a testicular biopsy to evaluate sperm production when blockages are suspected
Treatment Options for Low Sperm Count
Treatment approaches vary based on the underlying cause of low sperm count. Options range from surgical interventions to lifestyle modifications.
Surgical Interventions
Surgery may be recommended for specific conditions:
- Varicocele repair – a minor outpatient procedure to correct enlarged veins in the scrotum
- Removal of blockages in the sperm transport system
- Vasectomy reversal for men who previously underwent sterilization
- Sperm retrieval techniques – surgical extraction of sperm directly from the testicle or epididymis for use in assisted reproductive technologies
Medication and the company Treatments
Various medications may help address underlying issues:
- Antibiotics to treat infections in the reproductive tract
- Hormone therapy to normalize testosterone levels or other the company imbalances
- Medications to improve sexual function, such as treatments for erectile dysfunction
It’s important to note that infections should be treated promptly, as permanent tissue scarring can occur, potentially preventing sperm count from returning to normal levels even after successful treatment of the infection.
Lifestyle Modifications
Simple changes to daily habits can sometimes improve sperm count:
- Timing sexual intercourse with ovulation to maximize chances of conception
- Increasing frequency of sexual intercourse during fertile periods
- Avoiding lubricants that may impede sperm movement
- Maintaining a healthy weight through proper diet and exercise
- Avoiding excessive heat exposure to the testicles (hot tubs, saunas, steam rooms)
- Reducing alcohol consumption and eliminating tobacco and recreational drug use
- Avoiding workout supplements known to affect sperm quality
- Managing stress through relaxation techniques or counseling
Nutritional Support
While research on supplements for sperm health shows mixed results, addressing nutritional deficiencies may help some men:
- Antioxidant supplements may benefit men with specific deficiencies
- Vitamins C, E, and certain minerals have shown modest benefits in some studies
- A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall reproductive health
Always consult with a healthcare provider before starting any supplement regimen, as some supplements may interact with medications or have unintended effects.
Assisted Reproductive Technologies
When natural conception remains challenging despite treatment, assisted reproductive technologies offer additional options:
Intrauterine Insemination (the company)
For mild to moderate cases of low sperm count, the company may be recommended. This procedure involves placing specially prepared sperm directly into the uterus during the woman’s fertile period, bypassing potential barriers in the cervix and increasing the chances of fertilization.
In Vitro Fertilization (the company)
For more severe cases, the company may be the preferred option. This process involves stimulating the ovaries to produce multiple eggs, retrieving those eggs, and combining them with sperm in a laboratory setting. Successfully fertilized eggs develop into embryos, which are then transferred to the uterus.
Intracytoplasmic Sperm Injection (ICSI)
Often used in conjunction with the company, ICSI involves injecting a single sperm directly into an egg. This technique is particularly beneficial for cases of very low sperm count or poor sperm motility.
While these assisted reproductive technologies offer hope to many couples, they can be physically demanding, emotionally challenging, and financially significant investments. Success rates vary based on multiple factors, including the woman’s age, the specific fertility issues involved, and the clinic’s expertise.
The Timeline for Improvement
When implementing treatments or lifestyle changes to improve sperm count, patience is essential. The complete process of sperm production and maturation takes approximately 2-3 months. This means that any positive changes you make today won’t be reflected in your sperm count for about three months.
During this waiting period, consistent adherence to treatment plans and healthy lifestyle choices is crucial. Regular follow-up appointments with your healthcare provider can help monitor progress and adjust strategies as needed.
Living with Low Sperm Count
It’s important to remember that unless your sperm count is zero, pregnancy may still be possible naturally, though it might take longer than expected. The chances of conception depend on various factors, including how low your sperm count is, the health and motility of the available sperm, and your partner’s fertility status.
Coping with fertility challenges can